The Precision Behavioral Health Initiative @ Cornell Tech
aims to advance the role of precision technology in transforming behavioral health.
What is Behavioral Health?
Behavioral Health is the scientific study of the emotions, behaviors and biology relating to a person’s mental well-being and ability to function in everyday life. The term “behavioral health” encompasses all contributions to mental wellness, including substances and their abuse, behavior, habits, and other external forces.
What is Precision Technology?
Precision Technology is a model that captures, analyzes, and actuates on the needs of individuals to optimize decisions, treatments and practices for improved outcome. In the medical context, an intervention is customized to the individual patient and their context instead of a one-treatment-fits-all model.
Precision Behavioral Health (PBH) is focused on developing precision technology for behavioral health.
In the United States alone...

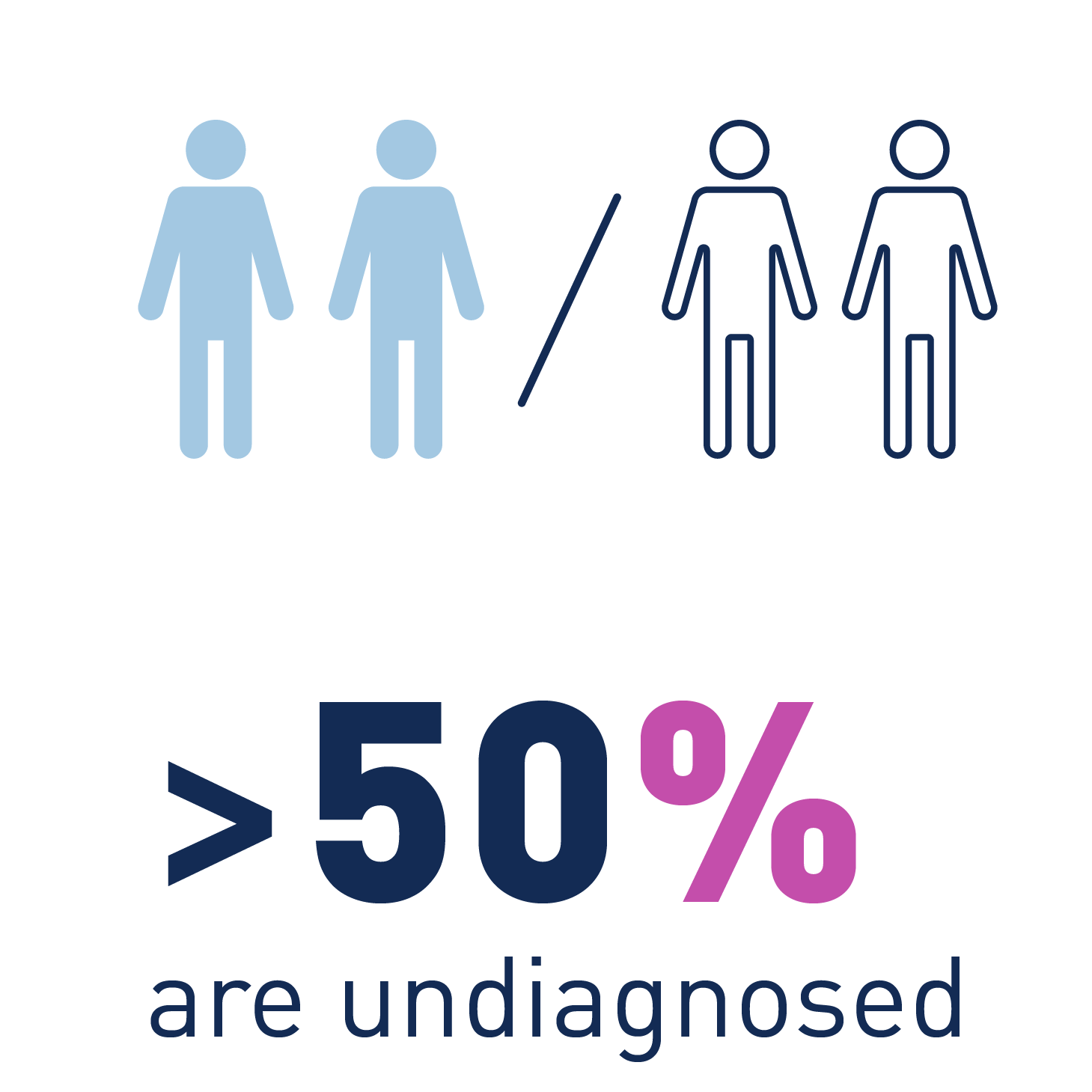

Even with more than 1000+ apps available and decades of research, these numbers have barely changed.
So why are tech advances not helping? We believe the problem lies in three critical gaps we need to overcome.
The Measurement Gap
Accurate, continuous, and longitudinal measurement of behavior is critical for successful treatment and recovery. Novel sensors on smartphones, wearables, and IoT devices have enabled detailed behavioral measurements within an individual’s day-to-day environment, reducing the need for patients to partake in lab-based studies or take on burdensome and unreliable self-reporting tools. These novel technologies have made it possible to continuously measure physical activity, sleep, sociality, physiological changes, mobility, mood, and much more -- however, the troves of data they generate are often too overwhelming for patients or physicians to use in clinically meaningful ways. Key to bridging this gap is attention to data actionability and privacy: we need AI models that balance interpretability with users’ privacy and security.
The Intervention Gap
Clinically grounded digital interventions (e.g, apps for cognitive behavioral therapy) mostly follow a one-size-fits-all protocol and do not leverage continuous behavioral measurements. Tighter synchronization between measurements and interventions can lead to improved outcomes at a lower user burden. Additionally, these intervention technologies should amplify patient-clinician relationships, rather than replace them.
The Clinical Impact Gap
What's the point of all these technological advances if they are not being used? They must be integrated into existing workflows. By designing with deployment in mind through clinician collaboration, and by embracing iterative design processes, we can introduce technology-based interventions that improve clinical outcomes. But this is not without challenges: novel interventions will need to scale to disparate contexts within an evolving U.S. healthcare landscape, reduce the burdens that additional tools introduce to clinical care teams, and support privacy for patients and providers alike.